This article addresses some frequently asked questions about RA and encourage those experiencing symptoms to reach out to Dr McKinnon for evaluation and management.
What Triggers Lupus Flares and Symptoms?
Lupus flares can be instigated by a myriad of factors, including stress, exposure to ultraviolet (UV) rays, infections, hormonal changes, and certain medications. Recognizing and minimizing exposure to these triggers can help mitigate the frequency and intensity of flares.
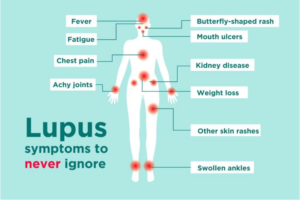
What Constitutes Lupus Symptoms?
The symptoms of lupus are diverse and can range from joint pain, skin rashes, fatigue, and fever to more severe manifestations like kidney dysfunction and neurological complications. Understanding and recognizing these symptoms are crucial for timely intervention and management.
How is Lupus Diagnosed and Treated?
Diagnosing lupus often involves a comprehensive assessment of symptoms, medical history, and laboratory tests to detect specific antibodies associated with the condition. Treatment approaches vary but commonly include medications to alleviate symptoms and modulate immune activity.
What are the Treatment Options for Lupus?
While there is currently no cure for lupus, traditional treatment aims to control symptoms, prevent flares, and minimize organ damage. Treatment plans are tailored to individual needs and may include:
Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, antimalarial drugs, immunosuppressants, and biologic agents may be prescribed to manage symptoms and suppress the immune system.
Lifestyle Modifications: Eating a healthy diet, exercising regularly, getting enough rest, avoiding stress can help manage lupus symptoms and improve overall well-being.
Monitoring and Regular Follow-ups: Regular medical check-ups and monitoring of lupus-related complications such as kidney disease, cardiovascular disease, and osteoporosis are essential for early detection and management.
Supportive Therapies: Physical therapy, occupational therapy, and counseling can help individuals cope with the physical and emotional challenges of living with lupus.
Integrative Care Strategies for Lupus Management:
Nutritional Support: Adopting a balanced diet can help support overall health and potentially reduce inflammation associated with lupus.
Mind-Body Techniques: Practices such as mindfulness meditation aid in stress reduction and promote relaxation, and improve overall well-being. Managing stress effectively is paramount for individuals with lupus to minimize flare-ups.
Physical Activity: Engaging in regular, low-impact exercise routines tailored to individual abilities can help improve joint mobility, muscle strength, and cardiovascular health.
Supplemental Therapies: Certain supplements may offer additional support for individuals with lupus.
Herbal Remedies: Some herbal supplements may offer adjunctive support in managing lupus symptoms. However, it’s crucial to exercise caution.
Empower Yourself with Knowledge and Support:
Living with lupus requires resilience, empowerment, and a strong support system. Educating yourself about the condition, advocating for your needs, and seeking support from healthcare providers, family members, and support groups can significantly impact your journey with lupus.
Connect with Dr. Naya McKinnon at Direct Access Rheumatology:
If you’re seeking comprehensive care and guidance for lupus management, consider reaching out to Dr. Naya McKinnon at Direct Access Rheumatology. Dr. McKinnon specializes in integrative approaches to autoimmune conditions, including lupus, and can work with you to develop a personalized treatment plan that addresses your unique needs and preferences.
In conclusion, navigating life with lupus requires a multifaceted approach that encompasses conventional treatments, integrative care strategies, and a proactive mindset. By embracing holistic principles of health and wellness, individuals with lupus can optimize their quality of life and cultivate resilience in the face of this complex autoimmune condition.

Gout
Have you ever had severe joint pain and wondered, “do I have Gout?” Now, you ponder what is the next step? This blog will cover the basics of Gout.

Beyond Medications: Diet, Meditation, Exercise, and Supplements
Our immune system protects our body from bacteria and viruses. Autoimmune conditions arise from dysfunctional immune system which can mistakenly attack its own tissues and organs. Although the exact cause of what causes the immune system to go haywire remains unknown, there are combination of factors which may play a role.

Understanding Hashimoto’s Disease: Frequently Asked Questions and How Direct Access Rheumatology Can Help
Living with Inflammatory Bowel Disease (IBD) can present numerous challenges, both physically and emotionally. The impact of IBD extends beyond the digestive system, often affecting various aspects of daily life. At Direct Access Rheumatology, we understand the complexities of managing IBD, and we’re here to offer support and guidance to individuals in the Las Vegas area.
Embracing Integrative Care: A Vital Approach to Managing Autoimmune Disorders
Living with an autoimmune disorder can be a challenging journey, one filled with uncertainty and varying degrees of discomfort. From rheumatoid arthritis and lupus to multiple sclerosis and Crohn’s disease, these conditions not only impact physical health but can also affect emotional well-being and overall quality of life.
Systemic Lupus Erythematosus (SLE): FAQs and Integrative Care Strategies
Systemic Lupus Erythematosus (SLE), commonly known as lupus, is a multifaceted autoimmune disorder affecting various organs and systems within the body. Understanding this condition is pivotal for those living with it and their support networks. Let’s explore some common queries about lupus and delve into integrative care methods for holistic management.

Living Life with Inflammatory Bowel Disease Arthritis Also Called Enteropathic Arthritis: 5 Steps for a Healthier Journey
Enteropathic Arthritis and Spondylitis is a specific form of arthritis associated with Inflammatory Bowel Disease (IBD) like Crohn’s and Ulcerative Colitis. This blog outlines five specific steps to navigate life with IBD arthritis.